Metabo-Oncology
The Cancer-Obesity Nexus
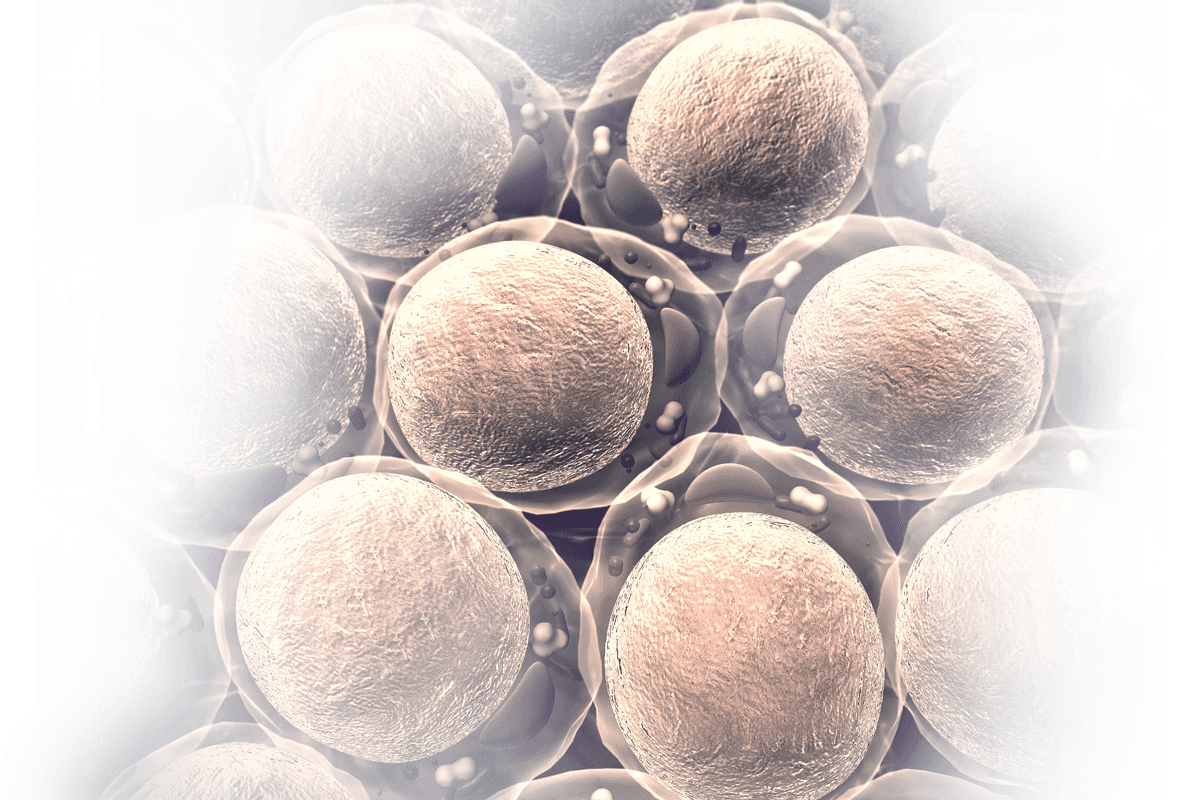
It’s a fact: Being obese or overweight raises the risk of developing certain cancers. Cancer patients who are obese or have metabolic dysfunction have more aggressive tumors, plus their metabolic state negatively impacts their response to treatment, including immunotherapies.
With rates of obesity, pre-diabetes and type 2 diabetes on the rise worldwide, addressing this problem is urgent.
Metabo-oncology is the emerging field of research focused on cancer patients with obesity or metabolic complications. This website is intended to enhance the medical and scientific communities’ understanding of metabo-oncology and share updates on clinical practices and the latest research.

For Doctors
Experience probably tells you that cancer patients with obesity/metabolic dysfunction don’t respond as well to cancer treatment as those without obesity/metabolic dysfunction. But do you know why — and what you can do about it? Find out what our experts have to say about this challenging patient population.

For Researchers
Cancer patients with obesity/metabolic dysfunction have a unique tumor phenotype due to their metabolic condition as well as distinct alterations in their immune system and tumor microenvironment. Research in this nascent field is developing a clearer understanding of the pathophysiology and etiology of metabo-oncology.
Expert Perspectives
Leading oncologists and researchers provide their insights on the emerging field of metabo-oncology, including the latest clinical developments and the current understandings in research.

Hope S. Rugo, M.D.
Medical Oncologist & Hematologist, University of California, San Francisco (UCSF) Helen Diller Family Comprehensive Cancer CenterLet’s say you have a patient who is over the target BMI. It would be great if you could say, “Here’s a medication you can take to address that, and here’s an exercise program that comes with it, and it has an app. We believe this will improve your response to therapy and your chance of survival, or at least your well-being.” That would be enormously appealing.

Kathryn H. Schmitz, Ph.D., MPH
Associate Director of Population Sciences, Penn State UniversityWhen we published recommendations on exercise oncology in 2010, we were trying to put the oncology world on notice that “rest, take it easy, don’t push yourself” is dead. Doctors need to be prescribing exercise for their patients during and after their treatment.

Neil M. Iyengar, M.D.
Medical Oncologist, Memorial Sloan Kettering Cancer CenterWhile the tumor-centric approach — where cancer prevention and cancer treatments are directed at the biology of the tumor itself — has been successful, we’re learning we can enhance this success by also focusing on the person as a whole and on what’s going on around the tumor. This is where metabo-oncology really becomes important, because the metabolic state of a person as a whole contributes quite a bit to how tumors develop and behave.

Andrew J. Dannenberg, M.D.
Professor of Medicine, Weill Cornell Medical CollegeThis is a global issue we’re dealing with. The epidemic of obesity, of excess adiposity, is here to stay. Therefore, finding strategies to alter tumor growth in those with excess adiposity is very important.