
About
About Metabo-Oncology
First it was chemotherapy. Then came targeted therapies. Now, immunotherapies are all the rage. Did you know that each of these therapeutic approaches is negatively impacted by obesity and metabolic dysfunction?
The next major advancement in cancer treatment is metabo-oncology, the area of research dedicated to understanding and treating cancer patients with obesity and metabolic dysfunction. This common co-morbidity centers on hyperadiposity (visceral fat) and metabolic dysfunction (e.g. insulin resistance, high leptin levels and chronic inflammation) which accelerate cancer growth and metastasis and protect cancer cells from immunosurveillance and many forms of treatment.
A Focus on Adipose (Fat) Tissue
Obesity is on the rise globally. Besides increasing rates of heart disease, diabetes and metabolic dysfunction, this trend puts people at greater risk of both getting cancer and dying from it. As reported in the Journal of Clinical Oncology:
“Obesity is associated with worsened prognosis after cancer diagnosis and also negatively affects the delivery of systemic therapy, contributes to morbidity of cancer treatment, and may raise the risk of second malignancies and comorbidities.”
Within the scientific and medical communities, there’s growing consensus that the key factors driving tumor growth and metastasis are:
- Excess visceral adipose tissue, which releases a variety of hormones and adipokines (signaling molecules from fat cells) that are stimulative to cancer
- Chronic, low-grade inflammation, which is associated with excess visceral fat and promotes insulin resistance
- Hyperinsulinemia, which is a known promoter of cancer progression, metastasis and mortality – even if the patient presents with normal glucose levels.
- Leptin, a fat-derived adipokine, is known to regulate energy metabolism and reproduction and to control appetite via the leptin receptor. Recent work has identified specific cell types other than adipocytes that harbor leptin and leptin receptor expression, particularly in cancers and tumor microenvironments, and characterized the role of this signaling axis in cancer progression. Emerging findings have demonstrated the direct and indirect biological effects of leptin in regulating cancer proliferation, metastasis, angiogenesis and chemoresistance, warranting the exploration of the underlying molecular mechanisms to develop a novel therapeutic strategy.

Metabolically Sensitive Tumors
Research has shown a link between metabolic dysfunction and worse outcomes for at least 10 types of cancer:
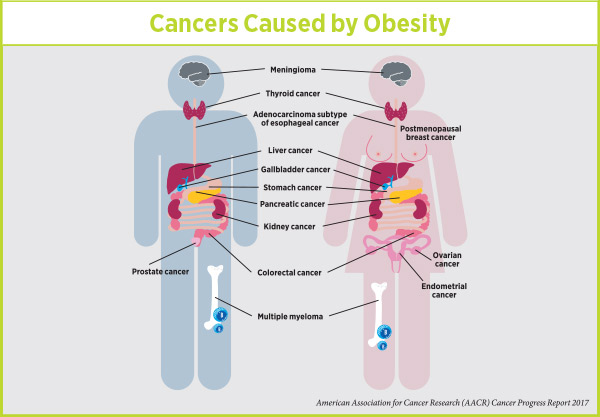
Posted on AACR website Jan 2018 by Karen Honey, PhD
These “metabolically sensitive” tumors constitute a significant percentage of all cancer cases in the United States, yet receive no special treatment. Furthermore, these patients have higher cancer mortality rates than their metabolically normal counterparts — as many as 84,000 cancer diagnoses each year are attributed to obesity, and overweight and obesity are implicated in 15% to 20% of total cancer-related deaths.
With an aging population and increasing obesity rates, the metabo-oncology problem is becoming more and more urgent. It’s time for action.